 |
| Discharge from cath number 8 |
 |
| Big sister got to come this time too |
School may have gotten out a week ago, but yesterday was our official first day of summer. Back in April, when we were told we'd need a cath in June, I carefully selected the date to be as close to the last day of school as possible. I couldn't possibly miss more time at work, but wanted to get the cath over with so that we could enjoy our summer. A summer away from the hospital. A summer without ouchies. So yesterday was that blissful first day. It was a stormy, rainy day, and in some ways I am grateful. I "slept in" until 7:15. We relaxed at home most of the morning then ran some errands and ate lunch. Both kids went down for a nap, or at least had quiet time in their rooms, my house is (mostly) clean, and I started catching up on my blog. It was pouring outside and so peaceful.
 |
| Playing in the waiting room at X-ray |
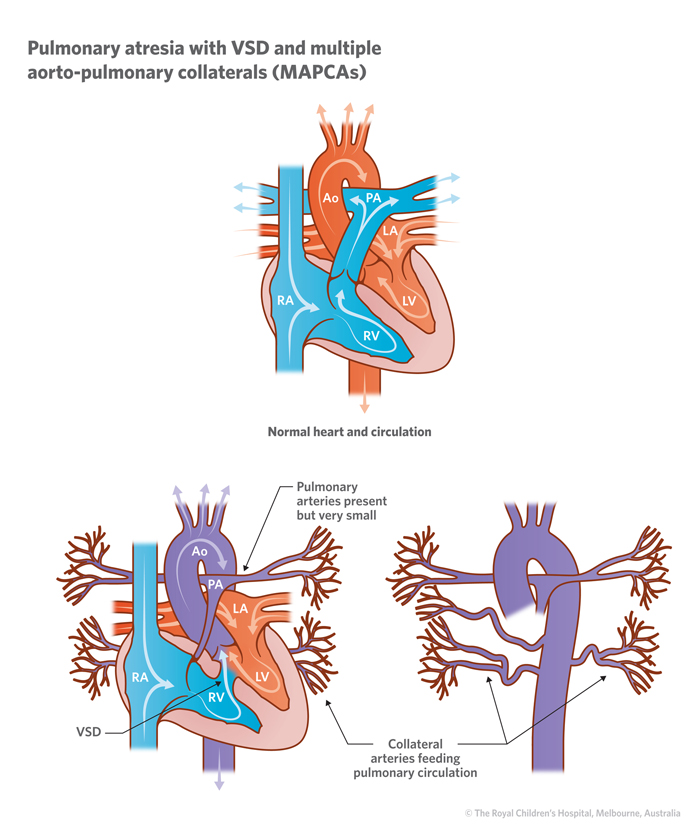
This was Reya's 8th catheterization. The first two were diagnostic, providing road maps for Dr Baird as he prepared to operate on her. The last 6 have been what is called "PA rehab" the PA standing for Pulmonary Arteries. This is the process of dilating / stenting Reya's MAPCAs (Major Aortopulmonary Collateral Arteries) and is the piece of Reya's diagnosis which necessitates all of these caths. In the human circulatory system, the pulmonary artery carries blood from the right side of the heart to the lungs. Both Reya and Hope were born with pulmonary atresia, which means the pulmonary artery did not connect the heart and lungs. The valve was there for both of them but was closed. In Hope's case, she was dependent upon the PDA (Patent Ductus Arteriosis) staying open. In the image below, that is the "vessel connecting the aorta and pulmonary artery". All babies are born with this (did you know blood flows differently in the womb?) and it closes up within hours of birth. In babies with Hope's birth anatomy, an open PDA is the only way that blood is going to get to the lungs to be oxygenated and then sent out to the body. This is why Hope required surgery so much younger than Reya. Without the MAPCAs, her repair was straightforward - placing a conduit from the right ventricle to the pulmonary artery, which eventually goes out the lungs, and closing the VSD. Her PAs were a decent size, so she did not require any dilating, and she has never had a cath.
 |
|
Reya, like Hope, has pulmonary atresia, but unlike Hope, she was not dependent upon her PDA. Instead, her body developed the MAPCAs off the aorta to allow blood to travel to the lungs. She was able to live like this for a while, but because of the VSD and the fact that the MAPCAs are coming off the aorta, the blood is mixed. This is why she has lived a good portion of her life with oxygen saturations in the 80s. This is not efficient and not sustainable. In addition to the mixed blood, her MAPCAs and her Pulmonary Arteries are very narrow, which is why she needs frequent caths and why she needed three surgeries before they were able to close off the VSD. The narrowness of her MAPCAs and PAs cause the pressures in her heart to be high, another reason why we couldn't close the VSD right away and instead had to focus on dilating the arteries to prepare for VSD closure. All of those caths eventually made it possible for Dr Baird to close the VSD this past April, but because the pressures were still relatively high, he had to leave a 4mm fenestration (a small communication hole) to help relieve the pressure and allow the blood to flow in between the chambers. We are told the hope is that eventually, her body will stop using this fenestration and it will eventually close off on its own. This cath was just another step in dilating the arteries and helping to lower those pressures. Here are a couple of diagrams. Click the link on the first one to see it bigger. Notice how small the pulmonary arteries are.
This time, because school was already out, Hope got to come along for the ride as well. She has been asking a lot of questions lately, and I felt like she needed to go to see what happens. She is a pretty anxious kid and I know she worries about Reya. It was not easy bringing them both. Pre-op is a long day - we arrived at 7:30 and didn't leave until almost 2. Both kids were pooped. Hope had a couple of meltdowns but mostly she was pretty good. In the aftermath this week, she has been a little difficult, claiming she is sick, telling me her belly hurts, etc. All of this a reaction to Reya's illness and hospital stay. Having the summer off will be so good for Hope.
 |
| Reya managed to sneak in a cat nap during her echo |
Neither kid got a real nap. Reya dozed during her echo and fell asleep in the car on the ride home, and even transferred to her crib, but didn't stay asleep long (she usually takes a 2-3 hour nap). Hope didn't nap at all all day. When we got home, I took them out to run some errands (literally) and both kids fell asleep about a mile in. They slept through our trip to Whole Foods and were still asleep when we got home. I felt about as tired as them and I did manage a nap while they were resting in their rooms.
 |
| Can you tell they're sisters? |
Our report time for the cath was 11:30. We haven't had this late of a report time before, at least not outpatient. In some ways it was nice - we had a pretty relaxed morning. Usually they try to get the littlest patients in first so that they don't have to wait around NPO (not allowed to eat). But with her case, we always require a back-up bed in the CICU. They were not going to have a back-up bed available for her early in the morning, so we had to come in later. They ended up calling us at 10:20 to tell us they were ready for us early. I was just getting out of the shower so I raced to finish up and head in. Chris would follow me a little later. We needed two cars since I would stay overnight and do discharge on my own the next morning. We have never been taken back so quickly. It is usually a hurry up and wait kind of thing, but this time, we went back right away, they took vitals, and then anesthesia was there with her little cocktail to help her relax. Chris arrived just in time to see her before she went back.
 |
| Mommy and Reya selfie! |
As most of you know, we have gotten really good at keeping ourselves occupied. It was a gorgeous day, so we decided to walk down to Fenway for lunch. It's a little under a mile. We had lunch at the infamous Cask and Flagon (where we watched the Sox win the 2004 World Series) overlooking Fenway Park. I hadn't been there in a long time, and I was actually really surprised by how good the food was! We spent the rest of the afternoon hanging out in one of the small gardens and then when there was enough shade, we went up to the new rooftop garden. I found myself really missing the Prouty Garden, which was always a relaxing place to hang out on a nice day. The new garden is nice, but does not have a lot of shade so it is pretty warm up there.


We said good bye to Reya around 11:30. We got updates every hour that she was doing well and around 5:30, we got a text from Dr Friedman asking if we were around so he could go over the results with us. He told us to meet us in the cath lab recovery room at 6, and by the time we got down there, she was back, so we were able to go sit with her. The cath was long - 5 HOURS, almost as long as her surgery, but incredibly successful. They were able to reopen the right femoral artery, which had been occluded. This is good news because it means we are able to use it again for future caths. It is bad news because we had to come home on Lovenox injections. 2x a day for a month. Not the best thing for a 22 month old, but if it saves the artery and gives them another point of access, I guess it is worth it. The were also able to dilate some of her vessels and they put a stent in as well, opening things up and relieving the pressures in her right ventricle. They were able to take the right ventricle pressure from 90 (which is really high, but not quite dangerously high) down to 60. RV pressure at 60 is still high for a normal person, but really good for a patient like her. We were told they aren't always able to get MAPCAs patients down that low. This bodes really well for her future. It means that it is possible that one day she will be able to play sports and do all the things a normal kid does. The most exciting thing of all was that today at the pediatrician, her sats were 96!
 |
| Out of the cath lab and looking pretty good. |
The down side to our later report time was that by the time we got up to our room, it was pretty late. I think we got up there around 7:30. After a cath, she needs to lay flat for 6 hours. This meant she was on bed rest until midnight. She was tired, but felt kind of restless from the anesthesia, so I had trouble getting her to rest. I finally got her to sleep around 11. Because of the right femoral artery situation, she needed a 6 hour Heparin drip and then her first Lovenox injection. When the Heparin ended, she needed a chest x-ray. Unfortunately, that ended at 2AM, so we had to go down to have a chest Xray at 2AM, as well as labs, and an injection. Our nurse, Tori, was great - while we were gone, she changed our linens (they were covered in orange popsicle) and turned Frozen on, creating a calm peaceful environment to come back to. Reya went back to sleep pretty quick, as did I. Unfortunately, we were woken up again at 6:45 by echo. It was not the most peaceful night, but what night in the hospital is? We ended up in a hallway bed, not a window, which I hate, but the monitor on the other side was broken, so we didn't get a roommate until late the next morning, after they had fixed the monitor, so that was nice. In the morning, we needed a lung scan and had to wait for them to sort out the Lovenox situation. We got to see a few old friends - Carole, the lactation consultant who had helped with both Hope and Reya, Ally, the nutritionist who has worked on our case multiple times, Lisa, the awesome case manager for the 8th floor, Susan, our NP from when she was inpatient post-op who cried when I showed her a picture of what Reya looked like healthy, as well as various nurses and staff. Everything was settled by about 12:30, but Reya had fallen asleep, so we decided to wait until she woke to discharge. We finally walked out the door around 2.
 |
| Enjoying her breakfast |
It was a successful cath and now we shouldn't need another intervention for the rest of the summer. Sadly, there are appointments, so we won't totally be left alone, but there aren't that many and they should be relatively quick. This is the 4th summer in a row where free weeks are taken up by doctor's appointments, though it is not quite as bad as the previous two summers were. She will not need another cath until NOVEMBER. Fingers crossed, but if everything goes well, this will be her longest stretch out of the hospital. We are really looking forward to the rest and relaxation the rest of the summer should bring. It has been a stressful 22 months, and just when we think things will settle down, something comes up. Maybe it is finally time.....











No comments:
Post a Comment